Pain with arousal
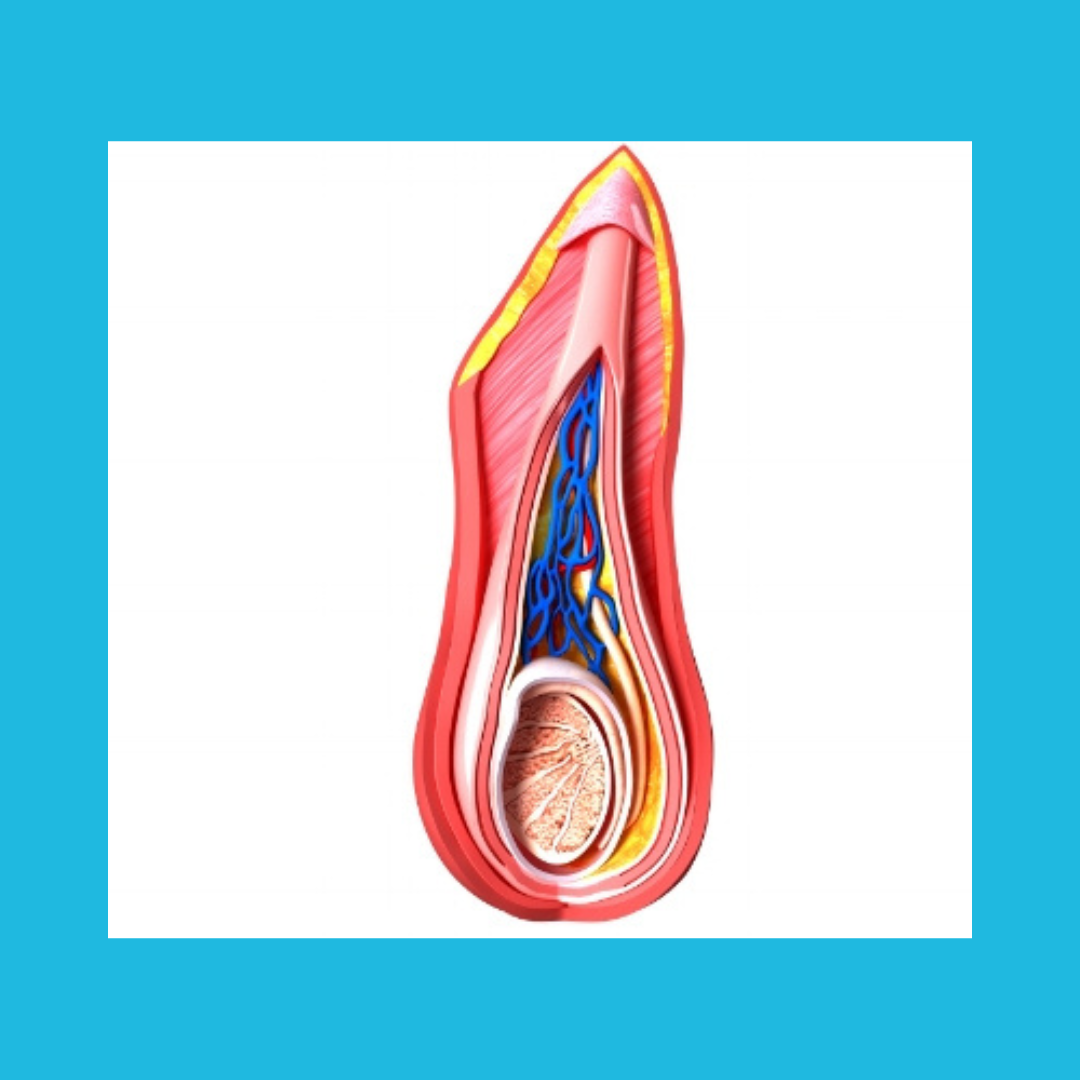
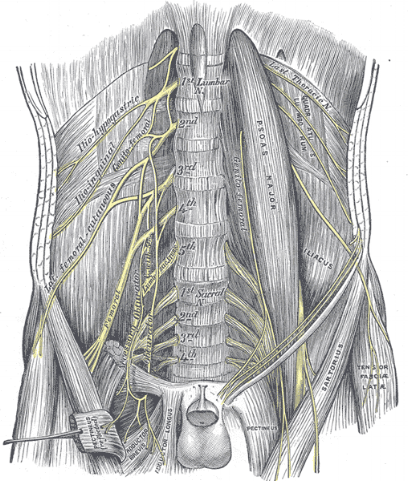
The mere physiologic function of having increased blood flow into erectile tissues (we’re talking about any gender here) can cause increased discomfort. Perhaps the muscles, nerves or tissues (including the vessels) are sensitive to any change in filling and pressure. Thinking about sex or feeling attraction can trigger such blood flow. This means that even a kind word whispered into a loved one’s ear or a gentle touch, even the thought of intimate acts can be painful. To emphasize this point, the pelvic area can become painful even before a person is ever touched.
Pain with orgasm or ejaculation
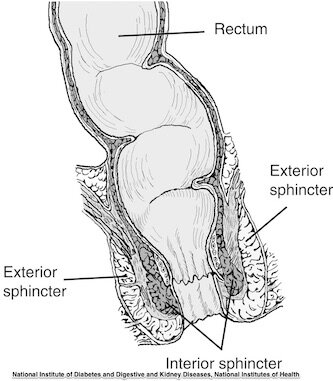
With pelvic dysfunction, achieving orgasm can be difficult due to muscle tension, changes in blood flow or physiology, or even due to fear and worry about performance or pain. Orgasm is often associated with ejaculation, and either often involve some really intense muscle contractions. If the muscles involved are painful, or if the nervous system is too sensitive, what should be pleasurable is excruciating. The rhythmic contractions that often characterize orgasm or ejaculation (remember that ejaculation is not for men only) can cause severe cramping, making it challenging for the person to want to engage in sexual activities, or to even avoid achieving climax.
Pain with positions limiting comfort
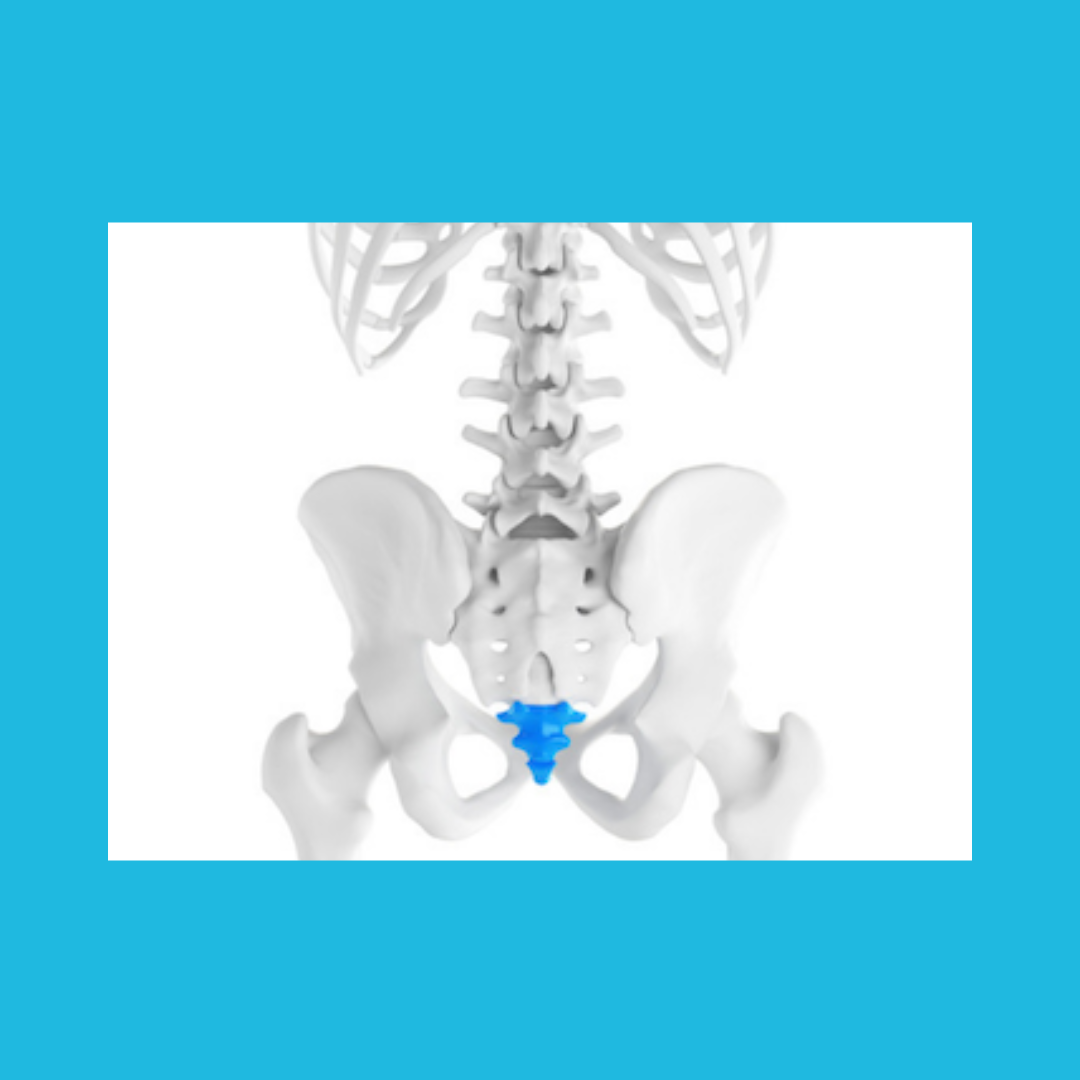
A couple’s usual positions for engaging in sexual activities (or even new positions) may cause activation of tender areas in the thigh, cause a cramp in the hip, or lead to aching in the back or pelvis. A severe case of sacral pain can make any prolonged position challenging to tolerate, and can feel worse with any added motion or weight. General orthopedic issues like arthritis, a joint replacement, a torn hip labrum, or tailbone pain can get in the way of lovemaking or sexual health.
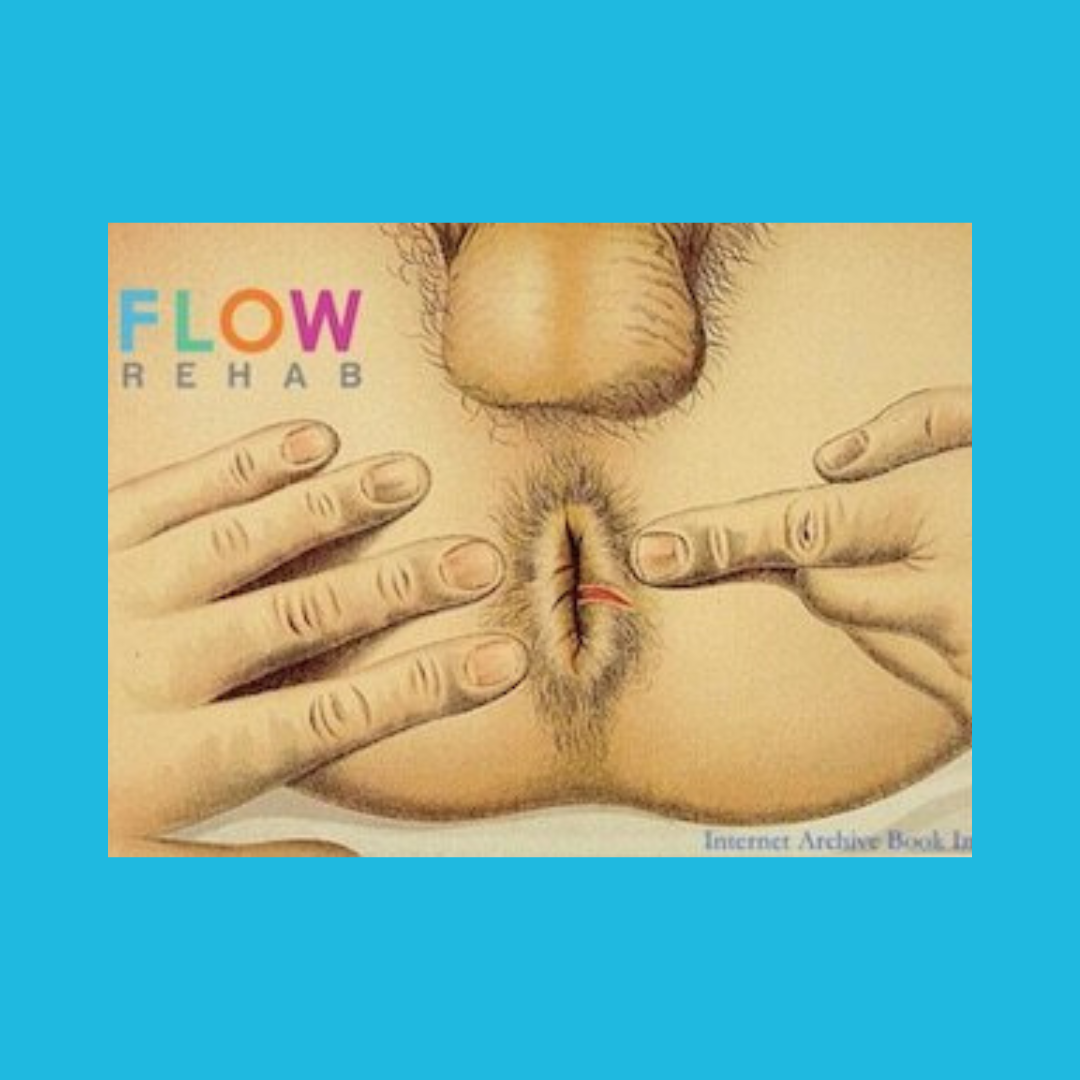
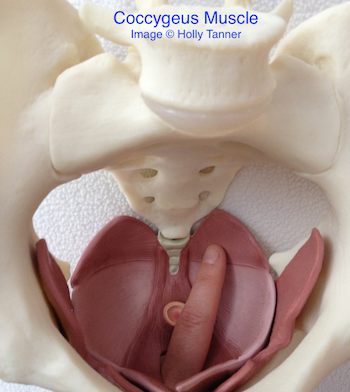
Pain limiting penetration
This is a really common problem. When the goal of the sexual activity is penetration of a canal, the opening or canal may be so tight, so tense, or so painful that the muscles and soft tissues do not allow for penetration. This can lead to frustration within relationships, more pain, avoidance of activity (or even avoidance of all sexual relationships) and may lead to harm if the person who has pain ignores the body’s tension. In the clinic it is not so unusual to meet a couple who has been trying to consummate a marriage for a very long time.
Pain following sexual activity
Even when sexual activity is tolerated, some people describe increased pain or cramping, aching, even burning for several days and sometimes 1-2 weeks after engaging in sexual activities. It’s no wonder that a person might give up on engaging in sexual health activities when these types of pain are present.
Pain limiting sexual health is very isolating, and not only within the relationship. Many of the people who come to the clinic describing limitations in sexual health think they are the only one to experience such challenges. When hearing that we in pelvic health work with people every day who have similar issues, this information can feel reassuring and hopeful. Some typical conditions that pelvic rehab specialists work with include sexual health following surgeries, in relation to cancer care, as part of healing pelvic pain, and for postpartum recovery. In all ages of life, from adolescent to adult, to older ages, all deserve to experience healthy and pleasurable sexual activities. This may include masturbation, or sex with a partner or partners, and the rehabilitation process may require a multidisciplinary approach. Knowledge from sex therapists or relationship counselors may be needed to bring about a return to healthy sexual activities.
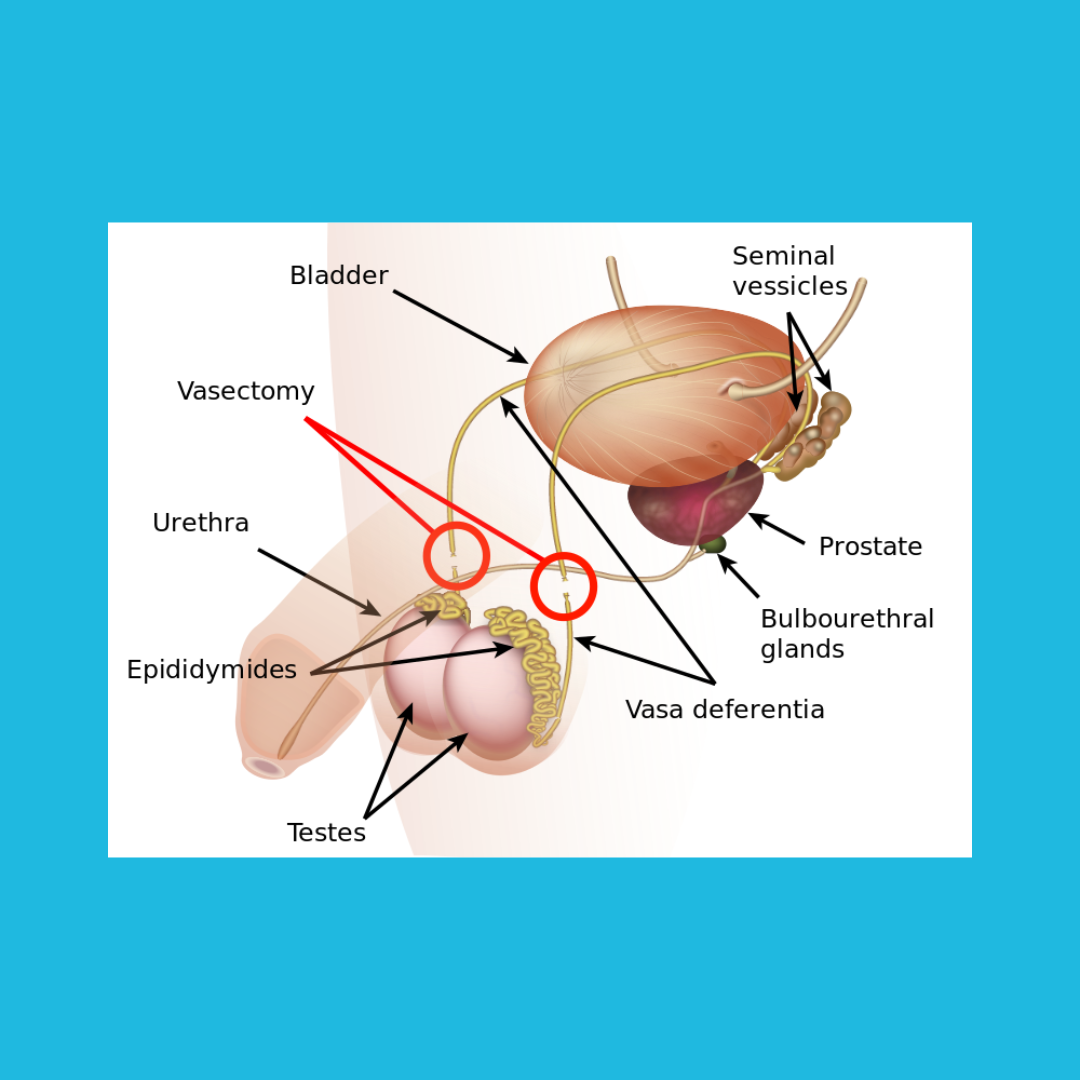
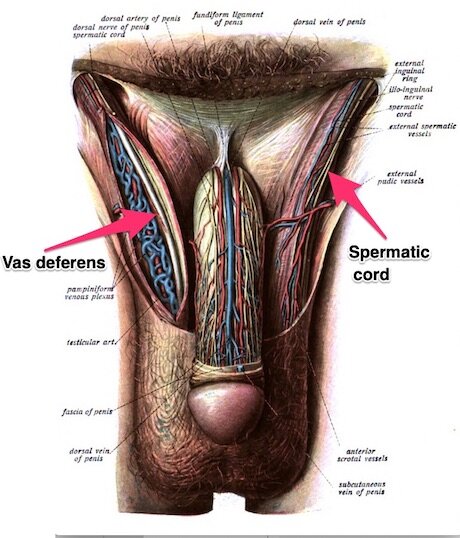
Although pain with sexual activities is common in cases of pelvic dysfunction, other issues can be going on. Sometimes lack of healthy blood flow, difficulty keeping blood flow into the erectile tissues, or difficulty getting the increased flow out of the pelvis afterwards is difficult. Some folks have low arousal, have issues related to hormones, and some have neurologic conditions that affect sexual health. As part of a team approach, pelvic rehabilitation is essential in helping people recover. If you have questions about the care that could be included in your recovery, find a local pelvic health therapist, and find out more about how to optimize your sexual health.